Occasionally, urban media carry a story about how some unfortunate seriously injured person was rushed quickly to hospital, only to sit unattended for a half hour.
Such incidents are undeniably cause for concern. But it would be helpful if, once in a while, the media noted that there is a class of Canadians who would love to have such speedy service.
They are rural Canadians, whose access to hospitals is sometimes measured in hours, not minutes.
They’ve seen rural hospitals closed in wave after wave of government spending cuts. Other health services have been “rationalized” to larger centres, and the loss of health-care facilities has made it more difficult to attract physicians to rural practice.
Read Also

Invigor Gold variety viewed as threat to condiment mustard
Invigor Gold, the canola-quality mustard developed by BASF, is on a collision course with Canada’s condiment mustard industry. It’s difficult to see how the two can co-exist.
Meanwhile, income taxes paid by rural residents continue to go into government treasuries at the same percentage rates urban Canadians pay. And the ever-increasing amount spent on farm inputs flows into urban economies, supporting hundreds of thousands of jobs.
The economic importance of farm input spending is worth emphasis. Few urban residents realize the revolution that has taken place over the past 25 years in agricultural production.
For example, at the time of the 1971 census Western Canadian farmers in total spent less than $17 million on pesticides. By the 1981 census, that had soared to $229 million, and by the 1991 census that had more than doubled to $509 million.
Rural areas, in short, more than pull their weight in contributions to the economy. Yet they receive far less in terms of health care and other social services. At one time, governments could point to the Crow transportation subsidy and other support payments as measures that somewhat offset rural disadvantages in services. But the Crow is gone, as are the days of big-ticket support programs.
No one expects the countryside to be dotted with major hospitals every 30 miles. But, with enough effort, surely ways could be found to stop the deterioration in rural services.
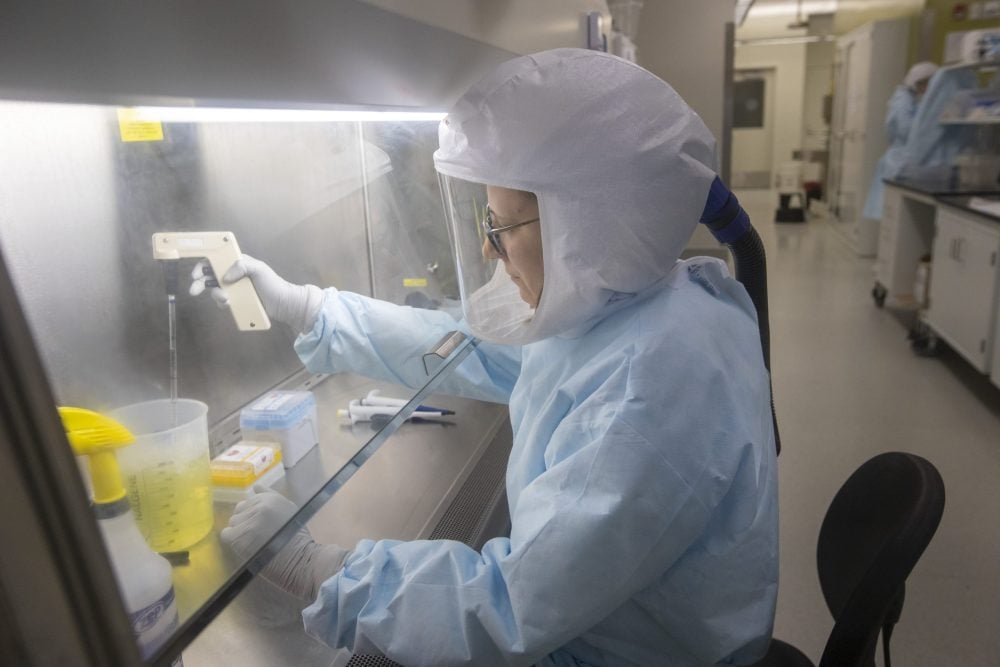
Reasonably priced solutions might be found in such areas as greater emphasis on paramedical personnel, use of remote diagnosis technology, mobile preventative clinics, and incentives for health-care professionals to work in smaller centres.
Improvements, however, will not be likely unless governments are pushed into making rural services a higher priority. As rural voting power declines, lobbying and public education become crucial. Rural and farm organizations have a key role here, and might usefully look for allies in enlightened businesses that profit from the countryside.